Hi all
STEMI equivalents can be tricky and a source of ED-Cardiology friction. I’ve gone through my collection to find some great examples, and I thought it might be a good idea to refresh some of the new kids on the block signs of coronary artery occlusion . click on the ECGs for big pictures.
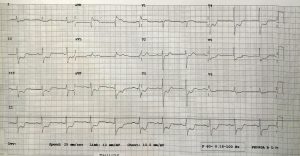
ECG 1:
This ECG is of a 39 year old man and clearly has STE in leadV 1-V3, although its the upsloping variety in V2-3. the TWs are huge – Fat – not skinny and thus not hyperK, they are classic hyperacute TWs. The TW in V4 is a classic DeWinters TW: a big TW with upsloping STD.
aVR shows STE and there is widespread STD.
Note aVL STE: this is a sign of a high lateral infarct as well, meaning there’s an occlusion proximal to the D1 (1st diagonal)
98% prox LAD at angio
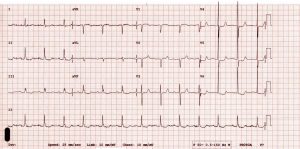
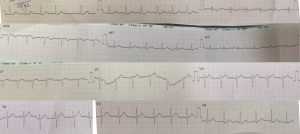
ECG 2
This ECG is of another young man (45) and shows the classic deWinters TWs (huge with upsloping STD) . Note the subtle but present STE in aVR and mild inf-lat STD. This guy had had a brief VF arrest before arrival. At eventual angio he had a 100% prox LAD .
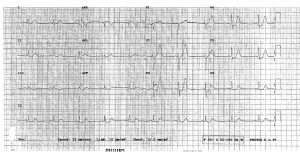
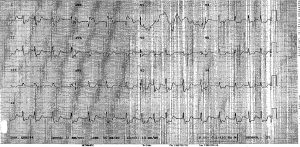
ECG 3
This is a 44 yo male with chest pain. He has hyperacute TWs (big and fat) with upsloping STE. This is not early repolarization for the following reasons. No J wave (notch) in R wave downstroke, no early R/S transition, big S wave in V3 (usually no S wave in V3). At the eventual angio he had 98% LAD
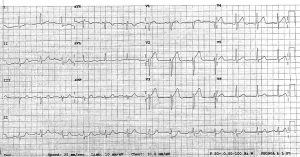
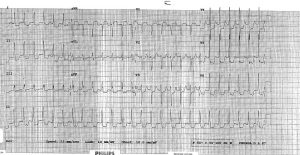
ECG 4
A more ‘bog standard’ aVR STEMI. Note the aVL STE which is the D1 territory from proximal LAD occlusion
ECG 5a
39 yo Sri Lankan male with central typical pain
next ECG shows the value of serials
ECG 5b
Taken to the lab by an excellent young cardiologist who was happy that these dynamic hyperacute TWs constituted LAD territory ischaemia. Prox LAD at angio.
ECG 6a
76 M with palpitations is this a STEMI?
ECG 6b
repeated after metoprolol led to sinus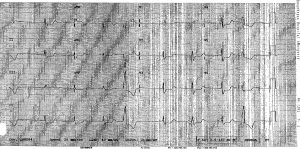
Persisting aVR elevation and STD after rate control, ongoing symptoms: cath showed LAD occlusion
ECG 7a
83F with palpitations, and a #NOF. Is this a STEMI?
ECG 7b
 Same patient now in sinus, shows classic LVH with ‘strain’or repolarisation abnormality. Flutter ECG shows the subendocardial rate related STD caused by a big ventricle suffering from a demand/supply issue
Same patient now in sinus, shows classic LVH with ‘strain’or repolarisation abnormality. Flutter ECG shows the subendocardial rate related STD caused by a big ventricle suffering from a demand/supply issue
DISCUSSION
aVR STE
aVR essentially ‘looks at’ the basal LV septum and is 180 degress opposite to to inf leads I and II.
So ST in aVR goes up if there is
1. Left main ( or LAD prox to LCx) occlusion ie STEMI where it means that the basal septum is having transmural ischaemia
2. When there is diffuse STD in the inferolateral leads (esp I,II,V5) , and thus is showing reciprocal STE to that STD (the STD which can be from any cause of myocardial insufficiency ie a supply demand issue – also called subendocardial ischaemia.)
Firstly a true Left Main (LMCA) STEMI is very rare in the ED, as most die before arrival. Having said that, in Sri Lanka, we saw heaps..including some in complete heart block , most of whom died in ED after lysis failure. aVR STE in these patients is a very bad prognostic sign .
Proximal LAD is more common and more survivable. Note the aVL elevation which supports this as it means that the first diagonal is occluded.
Secondly, the insufficiency causes, may be from:
a. NSTEMI (STD often horizontal) or
b. LVH (STD often down- or up-sloping, with repolarisation abnormality, most commonly when the patient is tachycardic). Fixed changes are seen also in bundle branch block (usually RBBB)
NSTEMI causing aVR STE can be from non occlusive Left main disease or , often, triple vessel disease if the STD is widespread. Here, the worse the disease, the more STD you get.
This amount of STD then can predict for bad outcome/ need to have CABG.
Remember that aVR is the reciprocal, so its amount of ST elevation in aVR is clearly going to also predict the above.
So to conclude with take home messages
1) In Non-STEMI, if there is STE in aVR more than 1.0 mm, it may be predict for Triple Vessels and CABG (Steve Smith (http://hqmeded-ecg.blogspot.com.au/ recommends withholding clopidogrel to not delay CABG)
2) In both STEMI and Non-STEMI, the degree of STE in aVR correlates with worse disease and worse outcomes; these patients should be referred for ASAP cath.
3) Patients with LVH and/or tachycardias may develop insufficiency related STD and RECIPROCAL STE in aVR: This may indicate they have coronary artery disease, but does not mean they need urgent intervention
deWinters T-Waves
These are hyperacute septal T waves with associated upsloping ST depression . They are also seen with mild (0.5mm) ST elevation in aVR, and are another STEMI equivalent. . About 2% of patients with LAD occlusion have these. They may progress into “full STEMI” but usually don’t improve. Thus they are different to Wellens (biphasic TW) and Hyperacute TWs that commonly evolve/resolve and usually don’t represent 100% occlusion.
Associated with younger, dyslipidaemic males – I wonder if this is because they commonly would have a single culprit lesion with better collateral supply and more resilient myocardium so they dont get the full transmural infarct STE pattern.
A New ECG Sign of Proximal LAD Occlusion N Engl J Med 2008; 359:2071-2073November 6, 2008DOI: 10.1056/NEJMc0804737
Verouden NJ, Koch KT, Peters RJ, et al.Persistent precordial “hyperacute” T-waves signify proximal left anterior descending artery occlusion. Heart. 2009;95:1701–6.
Hyperacute TWs
Here’s the detailed explanation of why these occur
“In the early phase of coronary artery occlusion the shortening of the subepicardial action potential (AP), resulting from activation of the ATP-dependent potassium current (I K-ATP), is thought to increase the endo-epicardial voltage gradient of repolarization, which, in turn, generates tall and peaked T waves. As the ischaemic insult prolongs, the epicardial AP dome may be completely lost leading to enhancement of transmural (i.e. endo-epicardial) and/or regional (i.e. from the surrounding healthy area toward the ischemic area) dispersion of repolarization and giving rise to the ST-segment elevation.15,16 Despite LAD coronary artery occlusion, the presence of collateral circulation may have provided subsidiary blood supply which saved epicardial myocardium from dying and prevented the classic ST-segment elevation pattern from occurring” (probably why its more often seen in younger patients)
Eur Heart J Acute Cardiovasc Care. 2012 Dec; 1(4): 344–348. doi: 10.1177/2048872612466537PMCID: PMC3760562 Interpretation of acute myocardial infarction with persistent ‘hyperacute T waves’ by cardiac magnetic resonanceAlessandro Zorzi
please add any comments, queries as usual below
Cheers









0 Comments
You can be the first one to leave a comment.